
Evidence Based Practice
Evidence-Based Practice, or EBP, is an important approach to clinical decision making used by healthcare teams and organisations worldwide. Nursing and Allied Health professionals with a good understanding of EBP are skilled to deliver care according to the best current evidence in a way that respects the unique circumstances and concerns of those receiving the care, their carers and families.
What is Evidence-Based Practice?
Evidence-based practice ‘requires that decisions about health and social care are based on the best available, current, valid and relevant evidence. These decisions should be made by those receiving care, informed by the tacit and explicit knowledge of those providing care, within the context of available resources’. [1]
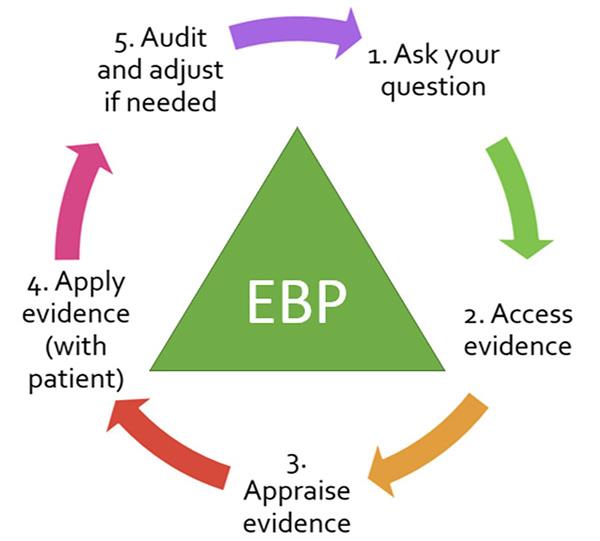
Clinicians frequently encounter gaps in their clinical knowledge triggering a need for information. EBP offers a structured way to finding a way forward when this occurs. The process is neatly summarised in the 5A model shown below.
This has five simple steps: Ask, Access, Appraise, Apply, and Audit.
Hold your cursor over each of the five steps to read more. If you can not see the interactive features of the diagram, you can view this information by accessing
The Five As of EBP (204kb PDF![]() ) information sheet.
) information sheet.
Audit
To close the loop, conscientiously evaluate the effectiveness of steps 1-4. This step is important as many clinical decisions will still have associated uncertainties, despite the availability of good quality evidence. An audit of patient outcomes will help you identify what you’ve learnt and what you might do differently next time. A less than optimal outcome might send you back to the Ask step again.
You get clearer answers when you ask clear questions. Start by turning a vague information need into a clearly constructed question. The easy-to-remember PICO mnemonic may help. PICO asks you to carefully consider and define the:
- Problem or population of interest in your question
- The Intervention (can be a therapy, diagnostic process, preventative or risk factor)
- Comparison intervention (if relevant)
- Outcomes of importance, both positive and negative, to you and the treatment recipient [2].
Access
Access the research literature using freely available reputable resources such as PubMed, Cochrane Library, PEDro (Physiotherapy), OTseeker (Occupational Therapy), speechBITE (Speech Pathology), or TRIP (Turning Research Into Practice). Seek relevant studies or syntheses of studies such as guidelines and systematic reviews. Do they focus on your PICO elements? If you have access to a health library, see what other resources are available to you, including librarian assistance.
Appraise
Critically assess the validity and applicability of the evidence found. There are checklist tools available to help you do this. These ask you to look at the methods used, the population studied, and the conclusions drawn. What does the evidence mean? How well was the study conducted? Were there biases in the process?
Apply
Consider the circumstances and individual preferences of the person you are seeking to treat. Is the person different in key aspects from the study’s participants, or close enough for the results to still apply? You may find a well-conducted study or synthesis, but its subjects may be younger, less debilitated, or in a different care setting. The study participants might be a good match, but the treatment may be too expensive or inconvenient. A treatment with potential health benefits may have significant side-effects. Ask for your patient's view of the evidence. Use your clinical expertise to incorporate their personal needs, goals, and preferences with the evidence to arrive at a joint decision.
What if there is no evidence?
Occasionally you may unable to find any empirical evidence to help answer a clinical question. This doesn’t necessary rule a treatment out. It will just require careful consideration and monitoring. In other words, "a lack of evidence does not equate to evidence of no effect" [3].
Why is there no evidence?
There may be strong ethical reasons why a study can't be conducted. Participation in a trial might cause harm to a patient. Researchers can't, for example, withhold potentially effective treatment from seriously ill patients in order to test a hypothesis. Clinical trials are also very expensive to run so certain treatments will naturally be prioritised over others for study.
References
- Dawes M, Summerskill W, Glasziou P et al. Sicily statement on evidence-based practice. BMC Medical Education. 2005; 5:
- Glasziou P, Del Mar C, Salisbury J. Evidence-based practice workbook: Bridging the gap between health care research and practice. 2nd ed. Carlton, Vic.: Blackwell Publishing/BMJ Books; 2007.
- American Speech-Language-Hearing Association [website] - EBP Process – Step 4: Make your clinical decision. Available from: https://www.asha.org/Research/EBP/Make-your-Clinical-Decision/ [accessed 3 Dec 2019]
Resources
Useful Websites
- American Speech Language-Hearing Association [website] - ASHA EBP resource for Speech Pathologists
- Collaborative of Australian and New Zealand Optometry Schools [website] - Evidence-based practice in Optometry
Video tutorials
- Duke Health [website] - Evidence Based Practice Series - Self-paced tutorials with interactive quizzes:
- Module 1: Introduction to Evidence Based Practice
- Module 2: Acquire: Finding the best evidence
- Module 3: Appraise: Therapy steps through the appraisal of a randomised controlled trial
- Yale University [video] - Framing questions with PICO [Vimeo Clip 4:11mins]
- Show me the evidence [video] - How to use the PICO method to form a clinical questions [YouTube Clip 2:58mins]
- Duke University Medical Center Library and Archives [Video] - A brief introduction to the hierarchy of evidence and study design [YouTube Clip 12:18mins]

